Are Sciatica and MS Related?
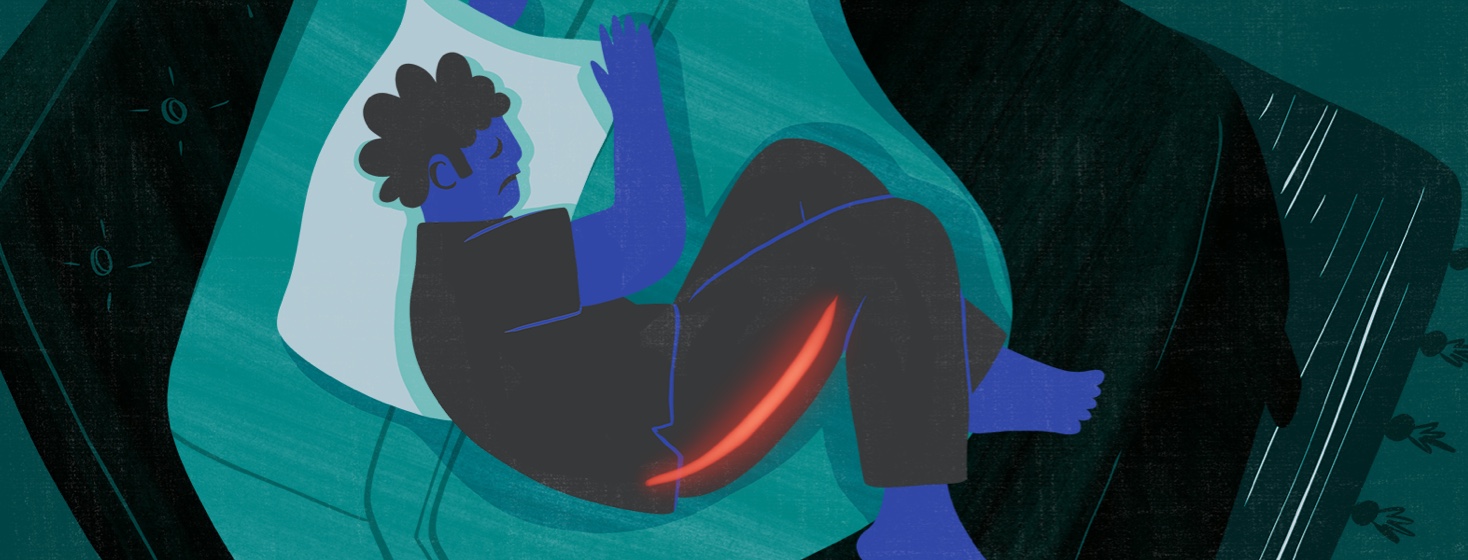
Sciatica is pain from an injured or irritated sciatic nerve. This is the longest, thickest nerve in the body. It starts in your buttocks area and runs down your legs into your feet. People with sciatica have mild to severe pain along the path of the nerve.1
Many people have sciatica, including some people with multiple sclerosis (MS). About 40 percent of people in the United States have sciatica at some point in their life. People who feel this type of pain may wonder if they have sciatica or MS. Some may think their sciatica is a symptom of MS.1
Experts once believed sciatica and MS were unrelated. But new research suggests there may be some links between the two.2
Symptoms of sciatica
People experience sciatica in different ways. Common symptoms of sciatica include:1,3
- Lower back pain, usually on one side of the body
- Pain that travels down the leg, typically one leg at a time
- Leg weakness
- A burning feeling in the buttocks
- A tingling or pricking feeling that goes along with the pain
- Pain that gets worse with movement
- Loss of movement
Several of these symptoms are also common in people with MS.4
Causes of MS pain versus sciatica
Both sciatica and MS can lead to pain. However, the main causes are different. This is because the 2 conditions involve different parts of the nervous system.1,5,6
Your body’s nervous system has 2 parts:7
- Central nervous system CNS – Your CNS includes your brain and spinal cord.
- Peripheral nervous system PNS – Your PNS is everything else. It includes nerves that travel from your spinal cord and brain to every other part of your body.
MS is considered a disease of the CNS. In people with MS, the immune system attacks the protective covering that surrounds nerve fibers in the brain, eyes, and spinal cord. This protective layer is called myelin. MS “short circuits” nerves that carry signals from the brain to the body.5,6
On the other hand, sciatica is not a disease of the immune system. The pain comes from direct pressure on the sciatic nerve, which is part of the PNS. Certain people are more likely to have sciatica than others. This includes those who have:1
- Herniated or slipped discs
- Diabetes
- Physically demanding jobs
- Osteoarthritis
Possible connections between sciatica and MS
For years, experts believed that MS affects only the CNS. However, some studies suggest that it also affects the PNS. For example, research has shown that people with MS have more damage to their sciatic nerves than those without the disease. This may mean the PNS is involved more often than experts once thought.2
More studies are needed to better understand how MS may impact the PNS, including the sciatic nerve. This could lead to new ways to diagnose and treat MS.2
Treatment for sciatica
Whether or not sciatica is related to MS, the condition can be painful. If you or a loved one has sciatica, speak to a doctor.
Fortunately, many people with sciatica get better with time and self-care. Treatment might include:1
- Icing
- Hot packs
- Over-the-counter drugs like ibuprofen
- Gentle stretching
If this does not provide relief, your doctor may recommend other options. They may include prescription drugs, physical therapy, and spinal injections. Surgery is not often needed. But your doctor might consider it if your symptoms do not improve within a year or so. Your care team can help you find the cause of sciatica and the best treatment.1
Join the conversation